Local News
Research reveals how newly formed neurons in the adult brain might repair motor circuits damaged by Huntington’s disease
Rochester, New York – In a significant breakthrough that challenges long-held assumptions about the human brain, scientists have discovered that the adult brain can generate new neurons capable of repairing damaged neural circuits—offering fresh hope for patients suffering from Huntington’s disease.
A new study published in Cell Reports reveals that the adult brain is not as limited as once believed. Under the right conditions, it can grow new, fully functional neurons that connect with existing brain networks—particularly those involved in movement, which are heavily affected in Huntington’s disease. This degenerative disorder gradually destroys nerve cells in the brain, severely affecting a person’s ability to move, think, and function.
“Our research shows that we can encourage the brain’s own cells to grow new neurons that join in naturally with the circuits controlling movement,” said Abdellatif Benraiss, PhD, senior author of the study and a research associate professor at the University of Rochester Medical Center (URMC). “This discovery offers a potential new way to restore brain function and slow the progression of these diseases.”
Turning Old Assumptions on Their Head
For decades, it was widely accepted that the adult brain could not regenerate neurons. Scientists believed that after early development, the brain’s capacity for creating new nerve cells essentially shut down. But new research has flipped that idea on its head. Specialized regions of the brain, such as the ventricular zone located next to the striatum, actually contain progenitor cells—cells that have the potential to become neurons.
In early development, these cells are active and produce many neurons. However, shortly after birth, they shift gears and mostly generate glial cells, which support the nervous system. But researchers have found that, under specific circumstances, these progenitor cells can be coaxed back into producing neurons.
The striatum, which plays a key role in coordinating movement, is one of the first areas of the brain to be damaged in Huntington’s disease. Replacing lost neurons in this area could be crucial to treating the condition.
How Songbirds Helped Crack the Code
The roots of this discovery stretch back to the 1980s, when scientists, including study co-author Steve Goldman, MD, PhD, were studying songbirds. These birds were found to regenerate neurons as they learned new songs, which led researchers to identify key proteins involved in the process—specifically brain-derived neurotrophic factor (BDNF) and another called Noggin.
Further research in Goldman’s lab showed that introducing BDNF and Noggin into the brains of mice stimulated the formation of new medium spiny neurons—the exact type of neuron that degenerates in Huntington’s disease. The team later demonstrated that this approach also worked in primates, strengthening the case for using it in humans.
Reconnecting the Brain’s Broken Circuits
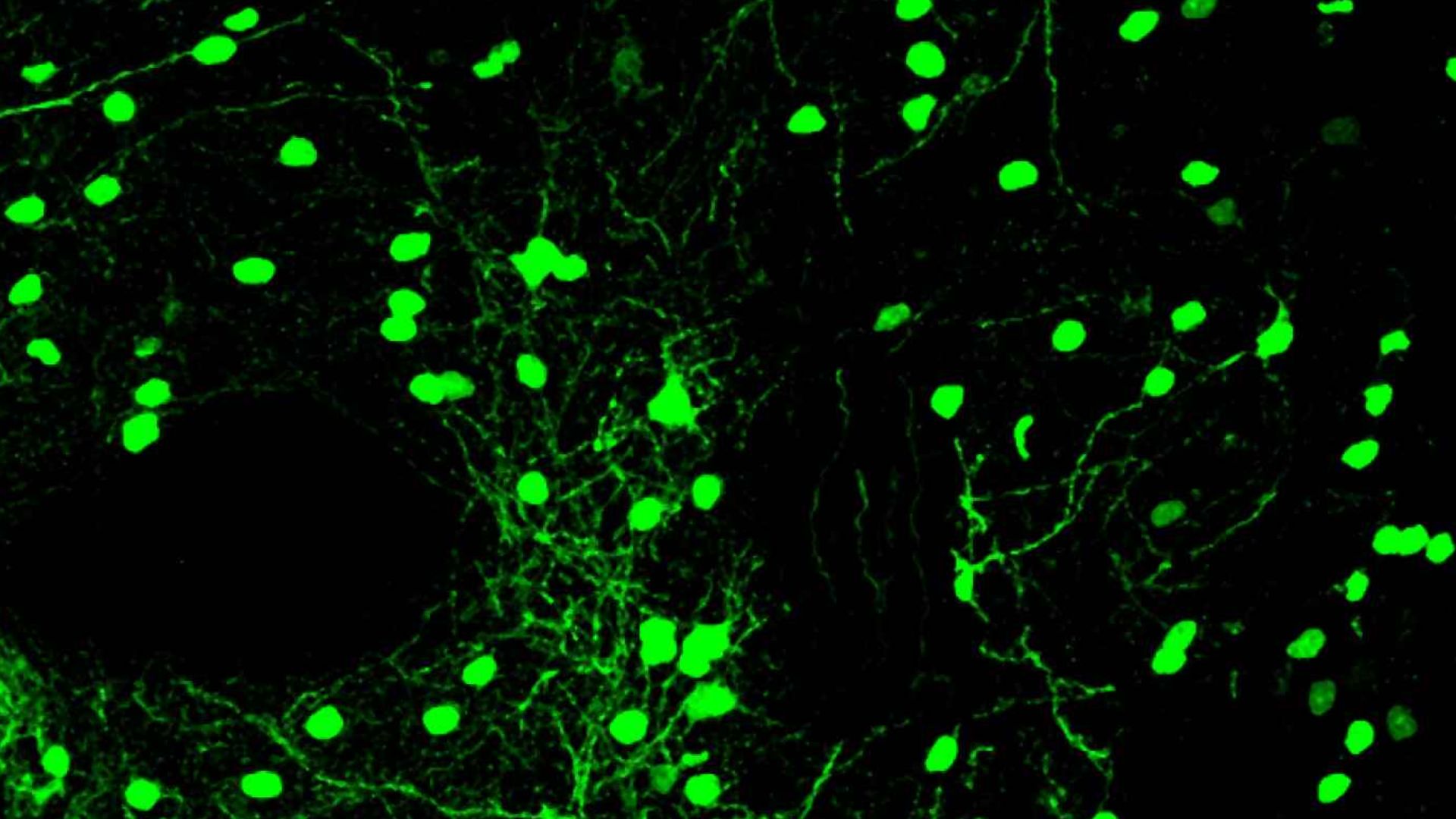
One of the biggest challenges was proving that these newly created neurons don’t just exist—they function. That’s what makes this latest study so groundbreaking. Using a mouse model of Huntington’s disease, the researchers marked the new neurons as they were created using a genetic tagging method. This allowed them to track the cells over time and observe how they matured and integrated into the brain’s complex motor networks.
“In this paper, we used a combination of electrophysiology, optogenetics, and mouse behavior to show that these cells are not only produced in the adult brain but functionally restore motor circuits in both healthy mice and in the context of Huntington’s disease,” said Jose Cano, PhD, lead author and postdoctoral associate in the Goldman lab.
Electrophysiology techniques enabled the team to measure the electrical activity of the neurons, while optogenetics—using light to activate specific cells—allowed them to switch these new neurons on and off. This helped confirm that the cells were actively participating in motor control and not just sitting dormant.
A Regenerative Approach to Treatment
The implications of this study are significant. If the brain can be prompted to regenerate its own neurons and rebuild lost connections, it could change the way neurodegenerative diseases like Huntington’s are treated.
“Taken together with the persistence of these progenitor cells in the adult primate brain, these findings suggest the potential for this regenerative approach as a treatment strategy in Huntington’s and other disorders characterized by the loss of neurons in the striatum,” said Benraiss.
Rather than relying solely on external treatments or transplanted cells, therapies might someday involve stimulating the brain’s own healing mechanisms to replace what’s been lost.
A Multi-Pronged Strategy
While the creation of new neurons is a major breakthrough, the researchers also believe it could be even more effective when combined with other therapies. One promising area of focus is glial cells, specifically astrocytes. These support cells are known to malfunction in Huntington’s disease and can disrupt normal brain function.
Goldman’s lab has previously shown that replacing damaged astrocytes with healthy ones in a mouse model can slow the progression of Huntington’s. This research is still in the preclinical stage but could one day complement neuron regeneration as part of a multi-faceted treatment approach.
Looking Ahead
Although this study was conducted in mice, the findings open a door to developing similar therapies for humans. The presence of progenitor cells in the adult primate brain is an encouraging sign, and researchers are hopeful that future clinical trials can explore this avenue further.
The study was conducted by a team at the University of Rochester Medical Center, with additional contributions from Cathryn Mangiamele and Maiken Nedergaard. Goldman and Nedergaard also hold appointments at the University of Copenhagen. The work was funded in part by CNS2, Inc., the Huntington Disease Golf Classic, and the Hereditary Disease Foundation.
While there is still much to learn, this research marks a powerful shift in how we understand the brain’s potential for self-repair. By reigniting the brain’s dormant ability to create and integrate new neurons, scientists are moving one step closer to finding real solutions for neurodegenerative diseases that once seemed unstoppable.
And that may be the most hopeful note yet for patients and families facing Huntington’s disease.

-

 Local News12 months ago
Local News12 months agoNew ALDI store close to Rochester to begin construction in late 2025 or early 2026
-

 Local News12 months ago
Local News12 months agoRochester Lilac Festival announces exciting 127th edition headliners
-

 Local News10 months ago
Local News10 months agoCounty Executive Adam Bello and members of the county legislature celebrate exceptional young leaders and advocates at the 2025 Monroe County Youth Awards
-

 Local News10 months ago
Local News10 months agoThe 2025 Public Market Food Truck Rodeo series will begin this Wednesday with live music by the Royal Bromleys